Diabetic Foot Ulcer Treatment in St. Johns County — Causes, Diagnosis, Treatment & Prevention
Diabetes is a long-term condition affecting millions worldwide, and it can impact many aspects of health. One of the most concerning complications is diabetic foot ulcers (DFUs). These wounds can start small but, if left untreated, may lead to serious infections, amputation, or even life-threatening complications. If you live in St. Johns County and are managing diabetes, knowing how to recognize, treat, and prevent foot ulcers is crucial. This guide will walk you through everything you need to know, from early warning signs and diagnosis to home care, advanced treatments, and prevention strategies.
What Is a Diabetic Foot Ulcer?

A diabetic foot ulcer is a chronic wound that develops on the feet of people with diabetes. It usually occurs due to a combination of nerve damage (neuropathy), poor circulation (ischemia), or consistent pressure on specific areas. Unlike regular cuts or scrapes, diabetic foot ulcers can persist for weeks or months and are prone to infection.

Common locations include the soles of the feet, toes, and pressure points, especially near thickened nails or calluses. Visual signs include red or black tissue, pus, foul odor, or even deep wounds that expose bone in severe cases. Clinicians often use grading systems like the Wagner or University of Texas scale to assess severity.
Who Is at High Risk?
Some individuals are more likely to develop diabetic foot ulcers. Key risk factors include:
- Long-standing diabetes (more than 10 years): Nerve damage and poor circulation increase with the duration of diabetes.
- Poor blood sugar control (high HbA1c): Uncontrolled glucose slows healing and increases infection risk.
- Peripheral neuropathy: Loss of sensation can make it difficult to notice small cuts, burns, or pressure points.
- Peripheral arterial disease / poor circulation: Reduced blood flow slows healing and increases ulcer risk.
- Previous foot ulcer or lower limb amputation: History increases chances of recurrence.
- Foot deformities: Bunions, hammertoes, or Charcot foot can create pressure areas prone to wounds.
- Calluses and thick nails: Add pressure that can break down the skin.
- Lifestyle and health factors: Smoking, obesity, kidney disease, older age, and poor vision.
- Limited access to podiatry care or low socioeconomic status: Less frequent checkups mean ulcers can go unnoticed.
Understanding these risk factors can help you take early preventive measures and seek care promptly.
How Ulcers Develop & “Spread”
Diabetic foot ulcers don’t appear overnight. They often follow a progression:
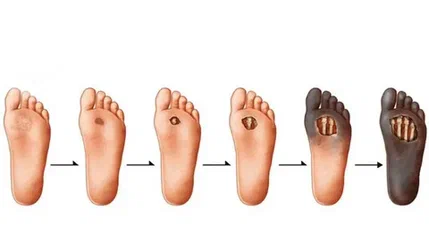
- Friction or small cut
- Development of a callus
- Skin breakdown leading to an open wound
- Local infection
- Deeper tissue or bone involvement (osteomyelitis)
- Severe complications like gangrene or sepsis
The two main drivers are neuropathy (so you don’t feel pain and detect wounds late) and ischemia (poor healing due to reduced blood flow). It’s important to note that DFUs are not contagious. “Spread” refers to progression within the body, not transmission between people.
Early Warning Signs
Recognizing an ulcer early can make all the difference. Watch out for:
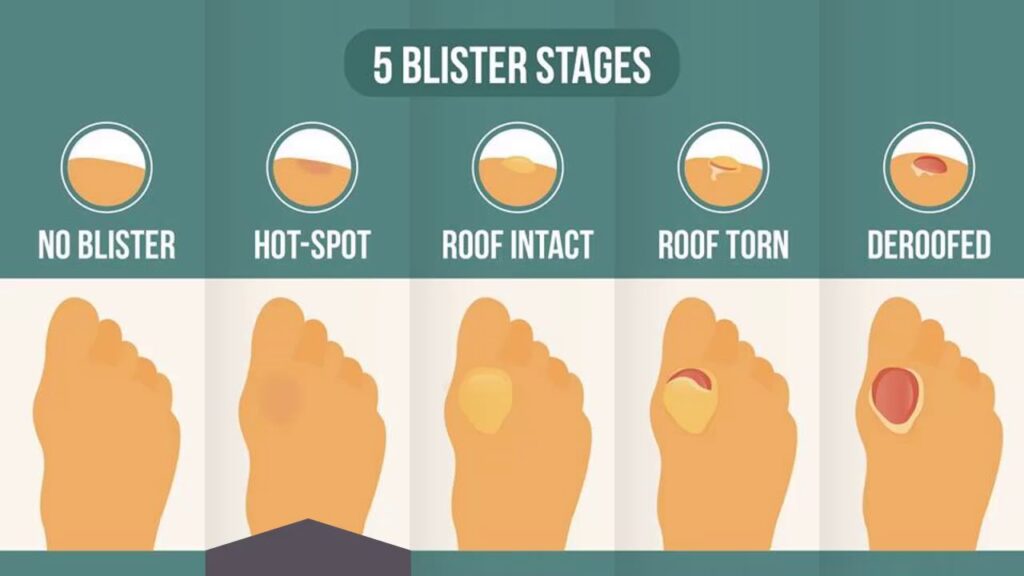
- New sores or non-healing blisters
- Redness, swelling, pus, or foul odor
- Numbness, tingling, burning, or loss of sensation
- Cool or pale skin, absent pulses
- Urgent red flags: spreading redness, fever, rapid pain, black tissue, or systemic symptoms
Tip: Avoid probing the wound at home — always let a trained clinician check it.
Diagnosis — Practical Checklist
Healthcare providers typically perform:
- History review: Diabetes duration, medications, previous ulcers, smoking, footwear habits
- Physical examination: Wound size, depth, margins, exudate, callus presence
- Sensory testing: Monofilament (10 g), pinprick, tuning fork
- Vascular assessment: Check pulses, ankle-brachial index (ABI), Doppler if needed
- Infection workup: Wound culture, CBC, CRP/ESR
- Imaging: X-ray for bone changes, MRI if osteomyelitis suspected
Documenting your wound with a dated photograph helps monitor healing over time.
Treatment — Step-by-Step Management
Immediate / First 72 Hours
- Clean the wound with normal saline and remove debris
- Apply sterile dressing; immobilize plantar ulcers
- Start antibiotics only if infection is present
- Off-loading: use a total contact cast or removable cast walker
Standard Ongoing Care
- Debridement: Regular removal of dead tissue
- Dressings: Maintain moist environment using alginate, foam, or hydrogel
- Glycemic control: Adjust insulin, monitor glucose, and maintain diet
- Infection management: Culture-guided antibiotics; hospitalize if severe
- Vascular interventions: Angioplasty or bypass if circulation limits healing
Advanced / Adjunctive Options
- Hyperbaric Oxygen Therapy (HBOT) for non-healing ischemic ulcers
- Negative Pressure Wound Therapy (NPWT) for large or post-op wounds
- Skin grafts, bioengineered tissues, or growth factor therapies
- Surgery: abscess drainage or partial amputation for non-salvageable tissue
- Multidisciplinary approach: podiatry, vascular, infectious disease, endocrinology, wound nurse
Follow-up Schedule
- Weekly for the first month, then biweekly based on healing progress
- Daily glucose monitoring
Home Care & Self-Management
- Daily inspection: Use a mirror or helper; take photos of any changes
- Cleaning: Mild soap + lukewarm water; dry between toes
- Dressing care: Follow clinician instructions
- Footwear: Never walk barefoot; always wear off-loading shoes
- Nail care: Professional trimming only
- Lifestyle: Stop smoking, eat protein-rich diet, take vitamins, and exercise to improve circulation
- Emergency: Call your clinic if there is drainage, new pain, fever, or color changes
Factors That Delay Healing
- Poor circulation or vascular disease
- Persistent high blood sugar
- Walking on the ulcer or ignoring off-loading
- Infection (MRSA, anaerobes, biofilm)
- Malnutrition or anemia
- Smoking or medications like steroids
- Social factors: limited clinic access, expensive dressings
Prevention — Stepwise Program
- Regular foot exams: every clinic visit; monthly for high-risk patients
- Daily self-checks and footwear inspections
- Routine podiatry care: callus removal, orthotics
- Maintain target HbA1c with clinician guidance
- Control comorbidities: blood pressure, lipids, kidney health
- Educate family and community for early detection
Complications & Prognosis
Potential complications include:
- Cellulitis, abscess, osteomyelitis, gangrene
- Partial or major amputation, sepsis
Prognosis depends on wound size, depth, infection, circulation, and glycemic control. Rehabilitation may include prosthetics or physiotherapy if amputation occurs.
St. Johns County — Local Action Items
- Seek urgent ER care if red flags appear
- Bring: glucose log, medications, wound photos, insurance
- Locate local podiatry/wound care clinics
- Verify insurance coverage for HBOT, home health, or off-loading devices
Patient Case (Example)
A 62-year-old man with 15 years of diabetes noticed a small blister on his big toe. Initially painless due to neuropathy, it worsened over two weeks. He visited a St. Johns County podiatry clinic, received debridement, off-loading shoes, and culture-guided antibiotics. Within six weeks, the ulcer fully healed, and he avoided amputation.
FAQs
- Is DFU contagious? No.
- Can it fully heal? Yes, with early treatment.
- When is HBOT needed? If standard care fails, after vascular assessment.
- Is surgery always necessary? Only in severe cases.
- How long does healing take? Weeks to months.
- Can I walk on the ulcer? No, off-loading is essential.
- Are home remedies effective? Avoid unverified remedies — consult your clinician.
- How often to visit a wound clinic? Weekly initially for non-healing ulcers.
Conclusion & Call to Action
Early detection, consistent monitoring, and multidisciplinary care can save your limb and improve quality of life. If you live in St. Johns County and suspect a foot ulcer, visit a podiatry or wound care clinic immediately, photograph the wound, and stop weight-bearing. Acting quickly is the key to successful healing.
Whats up guys! Want to say I stumbled upon this site 97pkr.info. Seems like it might be what I’m looking for, if you looking for this kind of info feel free to visit 97pkr.